Diabetic Retinopathy Specialists
Diabetic Retinal Disease
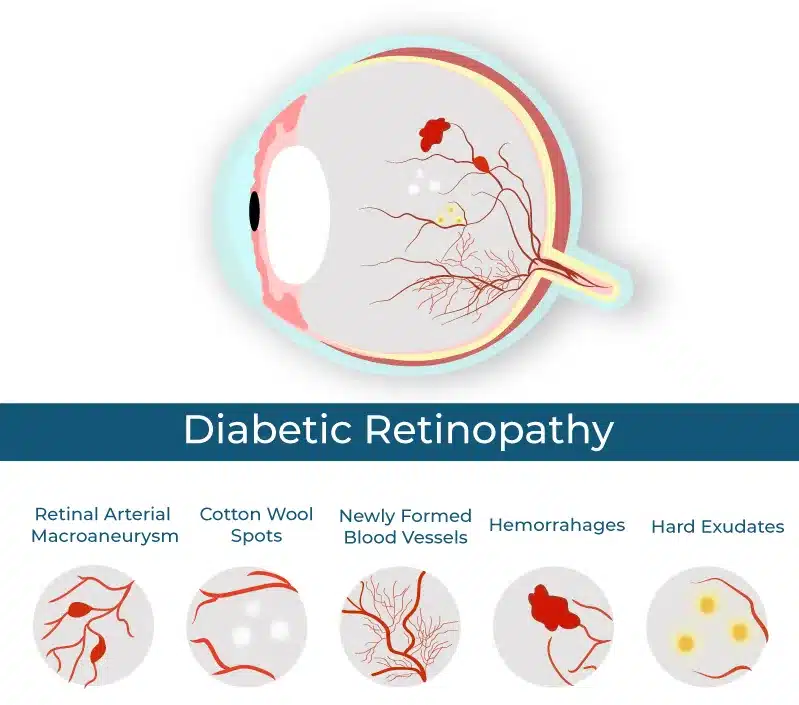
In patients with diabetes, the body does not store and use sugar properly. High levels of sugar in the blood can damage the tiny blood vessels throughout the body – in the heart, the kidneys, the brain, and the eyes. Damage to the blood vessels of the retina (the nerve layer at the back of the eye responsible for vision) is called diabetic retinopathy. Diabetic retinopathy can occur in anyone who has Type I, Type II, or gestational diabetes and is the most common diabetic eye disease. It is also the leading cause of blindness in American adults ages 20 to 74.
Retinopathy can cause severe damage to the delicate retinal tissues and cause both temporary and permanent vision problems. Those diagnosed with diabetes should not wait for the symptoms to appear, as there is no pain and vision may not change until the disease becomes severe.
Non-proliferative diabetic retinopathy
The first stage of diabetic retinopathy is called non-proliferative retinopathy (NPDR). A patient may have NPDR and have only mild blurring or no symptoms at all, even though significant damage to the retinal tissue is beginning. During this stage of the disease, portions of the retina’s blood vessels weaken and bulge outward; hemorrhages and microaneurysms result. Some of these unhealthy capillaries have very poor blood flow and are unable to deliver nutrients to the retina resulting in further damage (macular ischemia). Damaged blood vessels or areas of ischemia often leak fluid within the retinal tissue, causing the retina to swell. This swelling is called macular edema and may require treatment. Our retina surgeons employ the most advanced imaging system in the world to evaluate and image diabetic retinal disease.
Proliferative diabetic retinopathy
With worsening blood flow and retinal ischemia, the tissues will try to compensate by attempting to grow new blood vessels. The formation of these abnormal new blood vessels indicates a transition to proliferative diabetic retinopathy (PDR), the next stage of the disease. These new vessels tend to be irregular and very fragile. These new vessels (called neovascularization) often rupture and leak fluid and blood into the eye. Hemorrhage in the eye (called vitreous hemorrhage) results in blurred vision, severe “floaters,” and in some cases, near-total black-out of vision. It may take weeks, months, or even years for the body to break down and resorb the blood in the eye from a vitreous hemorrhage. Laser treatment and vitrectomy surgery could be needed for PDR.
Preventing Diabetic Retinopathy
Patients can protect their vision with continued annual eye exams, regular meetings with their physicians, and proper management of weight, blood sugar, blood pressure, and cholesterol management. Eventually, the mass majority of people with diabetes will develop eye disease; however, early detection can reduce the risk of vision loss by 95 percent, according to the National Eye Institute.
If diabetic retinopathy is detected early, it can be treated. An annual dilated eye exam will find signs of the condition, even if there are no symptoms. Research has shown controlling diabetes slows down the onset and progression of retinopathy, especially if blood glucose levels are well-managed. If a severe case is suspected, a physician may perform a fluorescein angiogram. A dye injected into the blood helps to view leaky or damaged blood vessels in the eye.
Diabetic eye issues can be detected during a routine eye exam. By dilating the pupil, an optometrist or ophthalmologist can visually examine the retina and other structures inside the eye. They can identify changes in blood vessels, leaky vessels or fatty deposits, macula swelling, and nerve tissue damage.
How Do You Treat Diabetic Retinopathy?
Diabetic eye issues can be detected during a routine eye exam. By dilating the pupil, an optometrist or ophthalmologist can visually examine the retina and other structures inside the eye. They can identify changes in blood vessels, leaky vessels or fatty deposits, macula swelling, and nerve tissue damage.
At Wellish Vision Institute, our retinal specialists will work with you and your unique vision needs to find the treatment options that are best for you. Diabetic retinopathy can be treated with medications and delicate surgical treatments, such as lasers.
- Photocoagulation: A laser is used to burn and seal blood vessels to stop blood from leaking and the vessels from growing.
- Scatter photocoagulation: The laser is focused in a polka-dot pattern by an eye care professional. Thousands of tiny burns are made during two or more treatments to shrink abnormal blood vessels.
- Focal photocoagulation: A laser is aimed at the macula to treat leaky blood vessels. The procedure keeps the blurry vision and other effects of macular edema from getting worse.
- Vitrectomy: A surgical procedure to remove scar tissue and the vitreous gel inside the eye. Vitrectomies are used to treat severe bleeding but can also restore vision and be used to reattach the retina.
Get Help Today
If symptoms of retinal diseases are making you uncomfortable and interfering with your daily life, call us. Our doctors have the expertise and tools to give you the relief you need.